No link was found between HPV vaccination and risk of autoimmune diseases in a study published in CMAJ
There is no increase in the risk of autoimmune disorders in girls who received the quadrivalent human papillomavirus (HPV4) vaccine.
Human papillomavirus is the most common sexually transmitted disease worldwide, affecting 50%-75% of sexually active people. The HPV4 vaccine is effective at protecting against 90% of the strains that cause cervical and anal cancer.
In India the highest technical body for vaccination has already cleared HPV vaccine for inclusion in the universal immunisation programme. However discordant voices continue to be heard questioning both the safety and efficacy of the vaccine.
Autoimmune disorders are diseases in which the body produces antibodies that attack its own tissues, leading to the deterioration and in some cases to the destruction of such tissue. Examples of autoimmune diseases include lupus, rheumatoid arthritis, type 1 diabetes, psoriasis, inflammatory bowel diseases and multiple sclerosis.
“Despite demonstrated effectiveness in real-world settings, concerns continue to persist regarding the safety of the HPV4 vaccine. In light of these concerns, we wanted to study the HPV4 vaccination since it was being offered free to all grade 8 girls in Ontario through school-based clinics,” says Dr. Jeffrey Kwong, a study author and a senior scientist at the Institute for Clinical Evaluative Sciences (ICES) and at Public Health Ontario. The study has been published in the Canadian Medical Association Journal.
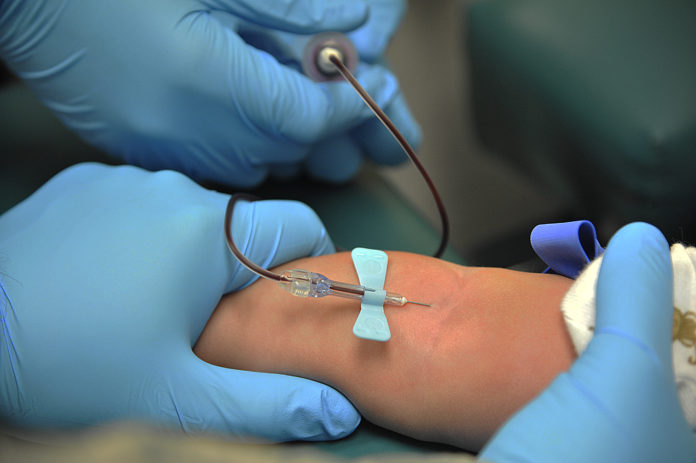
Researchers looked at data on 290 939 girls aged 12 to 17 years in Ontario who were eligible for vaccination between 2007 and 2013. Of the total 180 819 girls who received the HPV4 (Gardasil and Merck) vaccination in school-based clinics, there were 681 diagnosed cases of autoimmune disorders between one week and two months after vaccination. This rate is consistent with the general rate of diagnosed cases in this age group.
According to information given out by the US National Institutes of Health (NIH), Human papillomavirus (HPVs) are a group of more than 200 related viruses. Many of them can easily spread through direct sexual contact, from the skin and mucous membranes of infected people to the skin and mucous membranes of their partners. They can be spread by vaginal, anal, and oral sex. HPV is associated with more than 80 percent cervical cancers, though not all HPV infections go on to become cancerous.
Cervical cancer is the second most common type of cancer in females in India. According to the National Health Profile 2017, there were 97909 cases of cervical cancer in 2015. In 2013 the figure was 92,731. It is projected to go up to 104060 by 2020. WHO 2017 position paper on HPV identifies the primary target population as girls aged between 9–14 years, prior to becoming sexually active.
The National Technical Advisory Group on Immunisation (NTAGI), the apex technical body in India, that considers available scientific evidence on vaccines and advises the government, had recommended that HPV be included in the national immunisation programme in January 2018.
“These findings add to the body of evidence on the safety of the HPV4 vaccine and should reassure parents and health care providers,” said Dr. Linda Lévesque, Leslie Dan Faculty of Pharmacy, University of Toronto, Toronto, Ontario.