New guidelines for treatment of pulmonary embolism was published today by the European Society of Cardiology (ESC)
The European Society of Cardiology (ESC) Guidelines on acute pulmonary embolism were published online today in European Heart Journal. They were developed in collaboration with the European Respiratory Society (ERS).
Acute pulmonary embolism is the third most common cause of cardiovascular death in the World, after a heart attack and stroke.
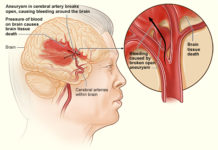
Pulmonary embolism occurs when a blood clot (thrombus) in a deep vein, usually in the legs, is dislodged and travels to the lungs where it blocks one or more vessels. This typically occurs if the vein wall is damaged, blood flow is too slow, or the blood becomes too thick.
The guidelines recommend how to judge the severity of pulmonary embolism based on a combination of clinical, imaging and laboratory results. This will dictate whether blood thinners alone are sufficient or if clot busters, a catheter intervention, or surgical removal is necessary.
Major surgery such as knee or hip replacement, serious injury, prolonged bed rest and cancer are common risk factors for acute pulmonary embolism. It can also happen after long travel and in women who are pregnant or taking the oral contraceptive pill.
“Symptoms including shortness of breath and chest pain resemble other diseases so the diagnosis is often missed, or the severity of the situation is underestimated, and many patients die before getting appropriate therapy,” said Professor Stavros Konstantinides, Chairperson of the guidelines Task Force and medical director, Centre for Thrombosis and Haemostasis, Johannes Gutenberg University Mainz, Germany.
The guidelines clarify how to diagnose acute pulmonary embolism step by step. The process begins with clinical suspicion based on symptoms combined with blood tests (D-dimers). Depending on the severity and urgency of the scenario, a computed tomography (CT) scan may be used to visualise the lung vessels, or cardiac ultrasound to look at the heart chambers.
A new table shows how CT scans and lung scans compare in their ability to diagnose or exclude pulmonary embolism, and how much radiation the patient receives with each of these tests.
Anticoagulant drugs (blood thinners) help the body dissolve clots and reopen the blocked vessels. If the patient is in shock and about to collapse, the clot must be removed immediately, and this can be achieved using thrombolytic drugs (clot busters), catheters, or surgery.
The guidelines recommend how to judge the severity of pulmonary embolism based on a combination of clinical, imaging and laboratory results. This will dictate whether blood thinners alone are sufficient or if clot busters, a catheter intervention, or surgical removal is necessary.
Advice for patients include :
-
Be aware of conditions that predispose to acute pulmonary embolism.
-
If you are at increased risk or have previously had pulmonary embolism or deep vein thrombosis, and are admitted to hospital for another disease, ask what is being done to prevent thrombosis.
-
If you have one or more risk factors for pulmonary embolism and feel shortness of breath, chest discomfort or chest pain, lightheaded or faint, call a doctor or ambulance immediately. Lie down and do not move around. Do not walk or drive to the hospital or physician’s practice.
-
If you had an acute pulmonary embolism and are on blood thinners, when you are discharged from hospital ask when you need to see a doctor again. At the follow-up visit, report any bleeding and whether you have returned to normal or still have symptoms such as shortness of breath.