A minimally invasive procedure called robotic stereoelectroencephalography (SEEG) increases accuracy of intractable epilepsy surgery
A new procedure called robotic stereoelectroemcephalography can make surgery for intractable epilepsy more accurate.
A study, published this week in JAMA Neurology, revealed that patients who had the minimally invasive evaluation procedure experienced fewer complications. Those who went on to have brain surgery were more likely to be seizure-free than patients who had the more invasive evaluation procedure.
Researchers reviewed 239 patients with medically intractable epilepsy who had a total of 260 procedures between 2004 and 2017 to locate the source of their seizures and determine their suitability for surgery. All procedures were performed at Memorial Hermann-Texas Medical Center.
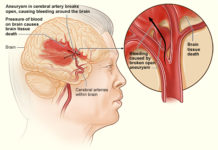
Of those 260 procedures, 139 cases involved traditional subdural electrode (SDE) implantation, which includes a large opening of the skull, known as a craniotomy. A sheet of electrodes is placed on the outside of the brain to pinpoint the seizure source before the skull closed back up for an observation period, which usually lasts around a week.
The minimally invasive technique also produced more favorable outcomes among patients with nonlesional epilepsy, for which surgery tends to be less successful
When the electrodes are removed, any surgery to treat the seizures is done at the same time to avoid having a separate craniotomy.
Another 121 cases involved robotic stereoelectroencephalography (SEEG), where electrodes are implanted via fine probes, which results in minimal blood loss and less pain.
The probes, thinner than raw spaghetti, are threaded inside the brain through small holes in the skull and patients undergo a similar observation period. Following the electrode removal, patients are typically discharged from hospital and, if they are candidates, will return in a few weeks for surgery.
Of the patients who underwent resection or laser ablation to remove the lesion causing their seizures, more than three-fourths (76 percent) of SEEG cases were either free of disabling seizures or had them rarely at the one-year mark, compared to just over half (55 percent) of SDE cases.
The minimally invasive technique also produced more favorable outcomes among patients with nonlesional epilepsy, for which surgery tends to be less successful. Nearly 7 of 10 of SEEG cases (69.2 percent) had good outcomes at the one-year mark compared to just over a third (34.6 percent) of SDE cases. A greater proportion of SEEG cases were nonlesional epilepsy – 56.2 percent, as opposed to 28.8 percent of SDE cases.
Findings also showed SEEG patients required significantly less narcotic medication than SDE patients (356 and 201 milligrams of morphine equivalents, respectively). The minimally invasive procedure also took less time, with the average time in surgery at just over two hours (121.3 minutes) for SEEG cases compared to more than five hours (308.2 minutes) for SDE cases.
“The findings give new hope to epilepsy patients who may previously have ruled out surgery for various reasons,” said lead author Nitin Tandon, MD, professor in the Vivian L. Smith Department of Neurosurgery at McGovern Medical School at UTHealth.