43 years later the damage that forced sterilisations during Emergency did to India’s population control drive are yet to be undone
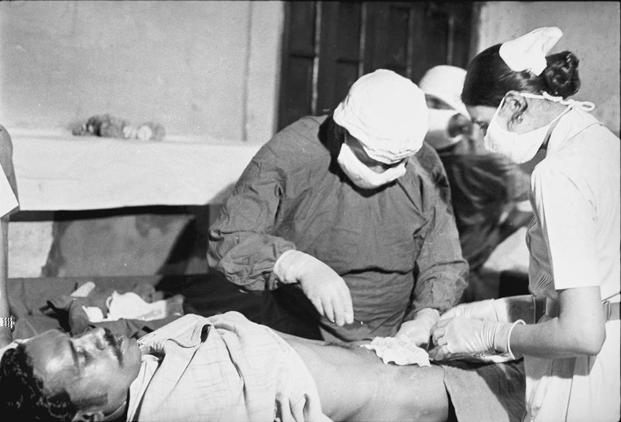
“And while a loudspeaker blared, there were figures descending from vans; a brightly coloured tent was being hastily erected, and there were camp beds and surgical equipment…” wrote Salman Rushdie in his description of the goings on in the magicians’ colony behind Jama Masjid during Emergency.
Saleem Sinai of course never recovered from the irreversible sterilisation that he was subjected to as a midnight’s child. Neither did India’s subsequent efforts at population control. This World Population Day as the world’s oldest family planning programme – India’s, that started in 1951 – grapples with the lingering fear that India may have already overtaken China as the most populous nation in the world, the Emergency scars refuse to heal.
That is why 41 years later in 2016, National Family Health Survey showed that of the 53.5% couples opting for “modern” birth control methods, 36% chose female sterilisation – by far the most complicated of all options. The least preferred was male sterilisation (0.3%) that earned a bad name during Emergency and has managed to hold on to that reputation for more than four decades. Meanwhile India’s annual birth cohort remains a staggering 2.6 crore babies. The total fertility rate (average number of children expected to be born to a woman during her lifetime) is 2.2. However of the 640 districts in the country, in 146 districts, the total fertility rate is more than 3.
Social stigma about males losing “strength” flourishing over decades, lack of male health workers to counter that subliminal propaganda and a system that is simply not ready for a rights based approach to population control is India’s biggest challenge
Though low uptake of male sterilisation is a global phenomenon, the disparity in India is particularly striking. A 2015 UN report on contraceptive use around the world said: “Male sterilization accounted for 10 per cent or less of all sterilizations among couples in 29 countries. There are, however, several countries where the prevalence of vasectomy equalled or exceeded that of female sterilization, ranging from 7 per cent male sterilization prevalence in Ireland to 22 per cent in Canada.” In the United States the most common contraceptive is the pill with 16% of all users opting for it. In Canada the percentage of pill users is 20.7, in the United Kingdom it is 28% and in Australia it is 28.8%.
To India’s defence – countries in the neighbourhood are more or less in the same bracket with the exception of Pakistan that has a TFR of 3.55. The TFR of Bangladesh is 2.14 and that of Nepal is 2.17. Bhutan is the only country in this part of the world that has managed to buck the trend. The Bhutan Living Standards Survey Report 2017 revealed that the country has achieved a total fertility rate of 1.9 – which means it is on its way now to population reduction.
Population reduction though is as much an issue of health as of society, as much about the choices available as people’s especially women’s right to make those choices. For 77% women undergoing sterilisation it is their first brush with contraception which shows that Indian women are still far from being able to make those choices freely. Female sterilisation is the most complicated option available.
In a bid to break, that trend, in 2017, India introduced injectable contraceptives into the family planning basket. Deoxymedroxy progesterone acetate (DMPA) is an injectable drug that prevents pregnancy by stopping ovulation – which is the release of an egg from the ovary. It does so by blocking the rush of Luteinising Hormone (LH) that causes ovulation. Unless that happens is is not possible for the egg and sperm to meet and form a zygote whose possible implantation makes a woman pregnant. It also makes both the processes of fertilisation and implantation more difficult. The data on its uptake is yet to come in.
But with social stigma about males losing “strength” flourishing over decades, lack of male health workers to counter that subliminal propaganda and a system that is simply not ready for a rights based approach to population control is India’s biggest challenge.


There is a new book on amazon.com titled From Malthus to Mifepristone: A Primer on the Population Control Movement by William Kay
https://www.amazon.com/Malthus-Mifepristone-Population-Control-Movement-ebook/dp/B07DNWS456