Health coaches, personalised glucose monitoring and incentives improve sugar levels in young children and teens with type 1 diabetes
A new pilot study which integrated caregiver coaching, personalized glucose monitoring and incentives into standard treatment in young children and teens with type 1 diabetes showed promising results. The study found that the children and adolescents manifested better control of HBA1c levels when compared to standard treatment alone.
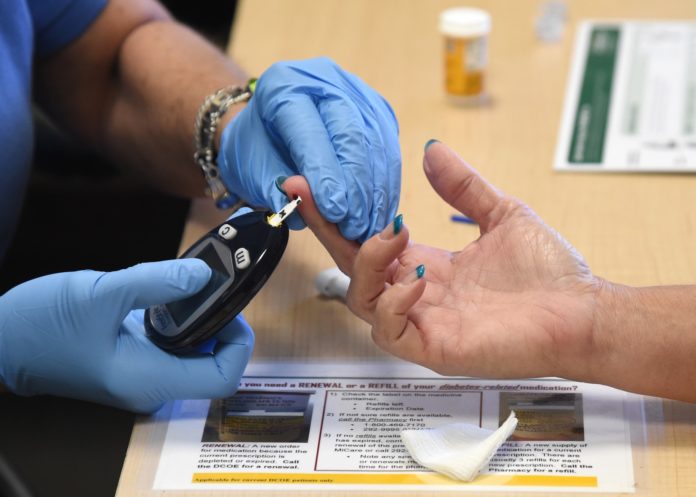
The life of a type 1 diabetes patient – taking daily insulin shots or wearing an insulin pump, monitoring blood sugar, prioritizing healthful food choices and fitting in daily exercise – can be challenging at age 5 or 18, creating challenges with compliance.
In this study, a team of diabetes educators, dietitians, social workers, psychologists and health care providers worked in tandem over a 10-week period to help families navigate care for children with type 1 diabetes.
Findings were presented at the American Diabetes Association’s 79th Scientific Sessions, at San Francisco.
“Teenagers aren’t always interested in long-term health outcomes, but they are interested in what’s happening right now. Fluctuating blood sugars can cause depression and problems with learning, while increasing risk for future complications, including eye problems, kidney problems and circulation problems.”
The pilot program included two components:
1. Weekly phone calls or emails from a health coach to a caregiver with personalized insulin adjustments, based on patient blood sugars submitted through continuous glucose monitoring apps; and
2. Incentives for patients to participate in the program and reach health targets.
Twenty-five participants, ages 4-18, with a mean age of 11.6 and A1c ranges between 8.6 – 10% joined the study. The average A1c was 9.4% at the beginning of the program and dropped by an average of .5% at the end of the trial. Twenty of the 25 participants, 80%, improved A1c levels by .5%. Seventeen participants, 68%, improved A1c levels by more than .5%, while seven participants, 28%, improved A1c levels by more than 1%.
“Chronic disease is like a marathon,” said Dr. Fran Cogen, M.D., C.D.E., director of diabetes care at Children’s National. “You need to have constant reinforcement and coaching to get people to do their best.”
Families who participated received a gift card to a local grocery store, supporting a child’s dietary goals. Children who participated were also entered into an iPad raffle. Improvements in A1c levels generated extra raffle tickets per child, which motivated participants, especially teens.
“These incentives are helpful in order to get kids engaged in their health and in an immediate way,” added Dr. Cogen. “Teenagers aren’t always interested in long-term health outcomes, but they are interested in what’s happening right now. Fluctuating blood sugars can cause depression and problems with learning, while increasing risk for future complications, including eye problems, kidney problems and circulation problems. As health care providers, we know the choices children make today can influence their future health outcomes, which is why we designed this study.”
Researchers will continue to study the impact of using this model over several months, especially for high-risk patients. Dr. Cogen concluded, “We’re moving away from office-centric research models and creating interventions where they matter: at home and with families in real time.”