Last year health budget went up by Rs 10000 crore, this time the hike is expected to be Rs 5000 cr taking the total health allocation to over Rs 52000 cr
India may get a 11% hike in its health budget. Top sources in the health ministry say that there are indications that a Rs 5000 cr increase may be in the offing when the Union Budget is unveiled next month.
Last year India’s health Budget after a Rs 10000 cr increase was a little over Rs 470000 cr. This year it is likely to be about Rs 52000 crore say health ministry officials. The figure is still way short of the 2.5% GDP health spend that the National Health Policy 2017 envisaged and has been a long standing demand of health experts starting from the High Level Expert Group on Universal Health Coverage constituted by the erstwhile Planning Commission to various international reports.
“We have managed to get our budget increases by Rs 5000 crore,” a senior health official said.
Meanwhile, for the first time the health ministry has also finalised a Rs 2000 crore plan for preventive healthcare, primarily screening for non communicable diseases. In its meeting last month, the Empowered Programme Committee of the National Health Mission approved Rs 1200 crore for NHM for 2018-19 and Rs 1600 crore for 2019-20 for comprehensive primary healthcare
It is a part of the upgrade of 153000 health sub centres into health and wellness centres as announced in the budget speech last year. Of this Rs 1200 cr will be a central allocation and Rs 800 crore will come from states’ kitty. This will mean that health sub centres whose sole function till now has been to provide ante and post natal care like vaccinations etc will for the first time be truly equipped to do basic health checkups for diabetes, hypertension, cardiovascular diseases and a few types of cancers and will also have a small basket of medicines available to be given to patients free of cost.
The growing burden of non-communicable diseases such as diabetes, hypertension and cancer is the most stark feature of India’s changing disease burden and experts have for long called for a comprehensive preventive model to tackle it. The National Health Policy unveiled last year too stressed on prevention and this is the first step in that direction.
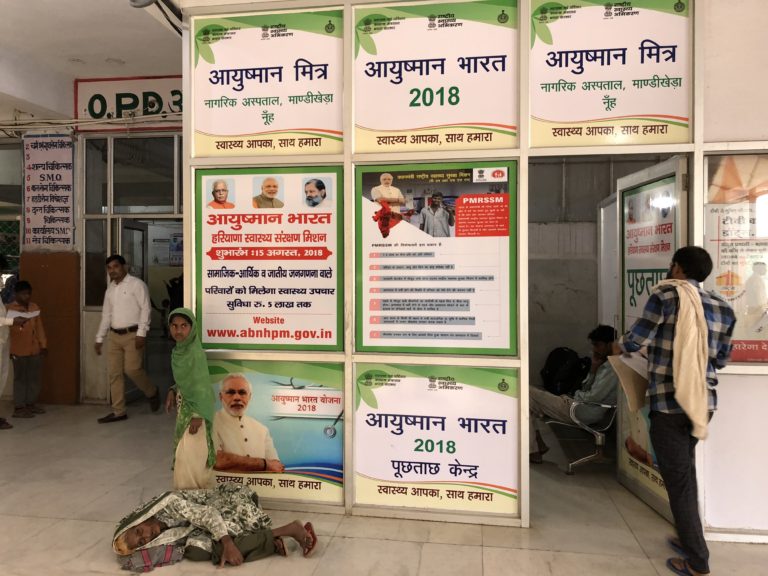
According to the blueprint drawn up by the Union health ministry, the new centres – to be called “health and wellness centres” would provide comprehensive maternal healthcare services to be
provided in those sites equipped to service as “delivery point”, comprehensive neonatal and infant health care services, comprehensive childhood and adolescent health care services, comprehensive contraceptive services, comprehensive reproductive health services, comprehensive management of communicable diseases, screening and comprehensive management of non-communicable diseases, basic ophthalmic care services, basic ENT care service, screening and basic management of mental health ailments, basic dental health care and basic geriatric health care services. The upgradation of each such centre would come at a cost of Rs 15-16 lakh and 500 centres across the country have already been approved. The target for the first year is 2500 centres