The tool that was developed using anonymised patient data from heart failure clinical trials has been made available free of cost
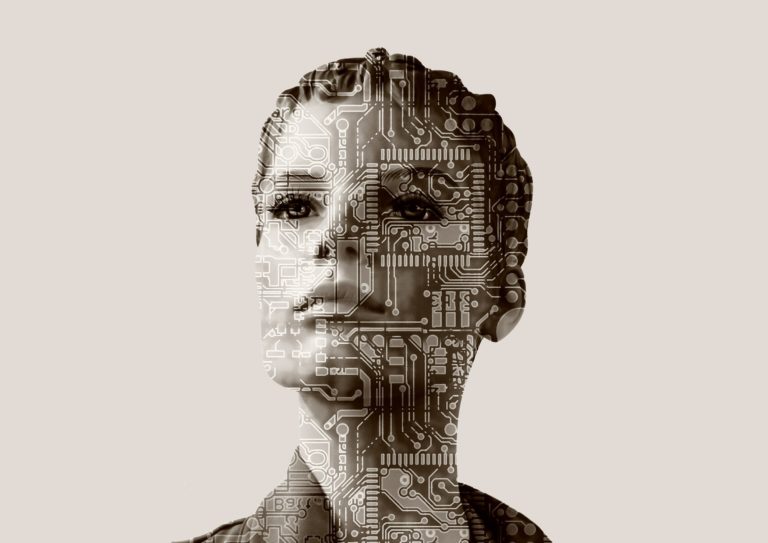
Researchers from the University of Virginia have developed a machine learning tool to analyse patient outcomes in people who have suffered heart failure. The tool is available free to clinicians.
Anonymised data from patients enrolled in heart failure clinical trials that were funded by the National Institutes of Health’s National Heart, Lung and Blood Institute. “This model presents a breakthrough because it ingests complex sets of data and can make decisions even among missing and conflicting factors. It is really exciting because the model intelligently presents and summarizes risk factors reducing decision burden so clinicians can quickly make treatment decisions,” said researcher Josephine Lamp, of the University of Virginia School of Engineering’s Department of Computer Science.
Heart failure is a condition when for reasons that can vary widely, the heart is not capable of pumping all the blood that is required for all functions of the body to be carried out effectively. It can lead to symptoms such as accumulation of fluids in vital organs. It is a condition that often required lifelong management and dramatic lifestyle changes, making immaculate and well informed medical decisions key to the care of such patients.
“The collaborative research environment at the University of Virginia made this work possible by bringing together experts in heart failure, computer science, data science and statistics. Multidisciplinary biomedical research that integrates talented computer scientists like Josephine Lamp with experts in clinical medicine will be critical to helping our patients benefit from AI in the coming years and decades,” said researcher Kenneth Bilchick, MD, a cardiologist at UVA Health. “