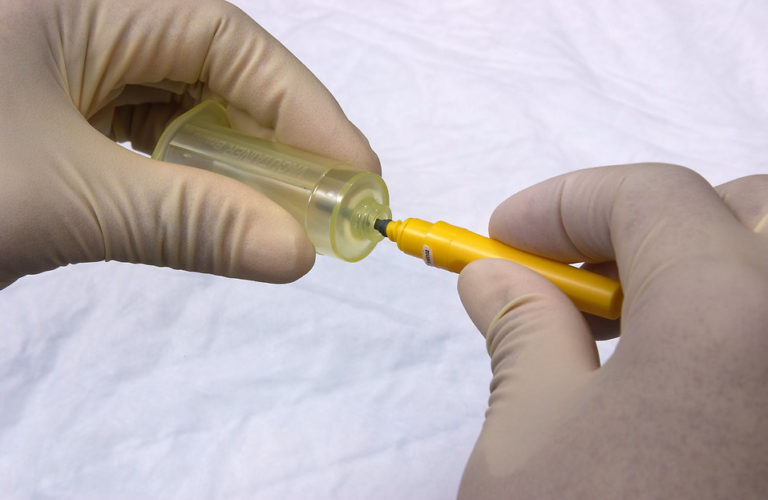
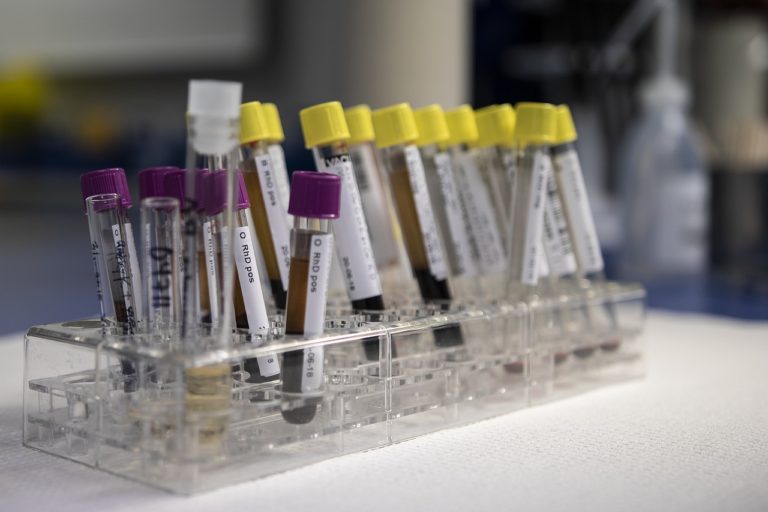
“Food Safety on Wheel” mobile lab, equipped with rapid testing kits capable of detecting 50 pesticide residues across various food matrices pressed into service

The Food Safety and Standards Authority of India (FSSAI) has launched an extensive awareness and sensitization program targeting major markets in the national capital, in collaboration with the Food Safety Department, Delhi.
Kicking off from the popular Khan Market and INA Market of Delhi on 8th April, 2024, the awareness campaign will focus particularly on the detection and mitigation of pesticide residue and contaminants in food products.
Market associations and traders were actively engaged and educated on the harmful effects of pesticide residue, mainly in fruits and vegetables and the importance of their testing. Additionally, attendees were introduced to FSSAI’s pioneering initiative, the “Food Safety on Wheel” mobile lab, equipped with various rapid testing kits capable of detecting approximately 50 pesticide residues across various food matrices, namely, fruits and vegetables, milk and cereals. Results from these tests are available within a few hours, facilitating swift action to ensure food safety.
Traders were encouraged to capitalize on this resource for expedited testing and to ensure the safety and quality of products sold in the market. Furthermore, they were also sensitized about a wide array of topics concerning food safety like the necessity of obtaining FSSAI licenses or registration and strict adherence to food safety standards. Traders were encouraged to source raw materials exclusively from FSSAI licensed/registered vendors to ensure traceability and compliance.
Further, the significance of raw material testing to guarantee the safety and quality of food products was emphasized during the programme. Awareness regarding artificial ripening and wax coating of fruits and vegetables using unapproved chemicals and role of organic farming was created among the attendees. Attendees were informed about the availability of testing laboratories for food products in Delhi and nearby areas.
The event emphasized the collective responsibility in ensuring food safety, with the mantra, “Food Safety is Everyone’s Responsibility” and also the importance of vital role of every stakeholder across the food supply chain in fostering a healthier India. FSSAI, as the apex food regulator in the country, remains committed to safeguarding public health through the implementation of robust food safety protocols nationwide.