 A study published in prestigious medical journal The Lancet has shown that a mere 10 kg weight loss and not the drastic reduction earlier thought necessary can reverse Type 2 diabetes. The late onset diabetes is usually caused by the body’s inability to use blood sugar lowering hormone insulin even though it is available.
A study published in prestigious medical journal The Lancet has shown that a mere 10 kg weight loss and not the drastic reduction earlier thought necessary can reverse Type 2 diabetes. The late onset diabetes is usually caused by the body’s inability to use blood sugar lowering hormone insulin even though it is available.
The study showed that after 1 year, participants had lost an average of 10kg, and nearly half had reverted to a non-diabetic state without using any diabetes treatment. “Our findings suggest that even if you have had type 2 diabetes for 6 years, putting the disease into remission is feasible. In contrast to other approaches, we focus on the need for long-term maintenance of weight loss through diet and exercise and encourage flexibility to optimise individual results,” says Professor Michael Lean from the University of Glasgow who co-led the study.
India is said to be the “diabetes capital” of the world. According to the World Health Organisation, India had 69.2 million people living with diabetes (8.7%) as per the 2015 data. Of these, it remained undiagnosed in more than 36 million people. Worldwide, the number of people with type 2 diabetes has quadrupled over 35 years, rising from 108 million in 1980 to 422 million in 2014. This is expected to climb to 642 million by 2040. This increase has been linked to rising levels of obesity and the accumulation of intra-abdominal fat. Bariatric surgery or gastric banding that is often used to treat morbid obesity or in a bid to control diabetes can cost around Rs 5 lakh.
“Rather than addressing the root cause, management guidelines for type 2 diabetes focus on reducing blood sugar levels through drug treatments. Diet and lifestyle are touched upon but diabetes remission by cutting calories is rarely discussed. A major difference from other studies is that we advised a period of dietary weight loss with no increase in physical activity, but during the long-term follow up increased daily activity is important. Bariatric surgery can achieve remission of diabetes in about three-quarters of people, but it is more expensive and risky, and is only available to a small number of patients”, explains Professor Roy Taylor from Newcastle University, UK, who co-led the study.[1]
The Diabetes Remission Clinical Trial (DiRECT), included 298 adults aged 20–65 years who had been diagnosed with type 2 diabetes in the past 6 years from 49 primary care practices across Scotland and the Tyneside region of England between July 2014 and August 2016. According to Professor Taylor: “Our findings suggest that the very large weight losses targeted by bariatric surgery are not essential to reverse the underlying processes which cause type 2 diabetes. The weight loss goals provided by this programme are achievable for many people. The big challenge is long-term avoidance of weight re-gain. Follow-up of DiRECT will continue for 4 years and reveal whether weight loss and remission is achievable in the long-term.”
Writing in a linked Comment, Professor Emeritus Matti Uusitupa from the University of Eastern Finland discusses whether these findings should change treatment options for type 2 diabetes. He writes, “Lean and colleagues’ results, in addition to those from other studies of type 2 diabetes prevention and some smaller interventions in this setting, indicate that weight loss should be the primary goal in the treatment of type 2 diabetes… The DiRECT study indicates that the time of diabetes diagnosis is the best point to start weight reduction and lifestyle changes because motivation of a patient is usually high and can be enhanced by the professional health-care providers. However, disease prevention should be maintained as the primary goal that requires both individual-level and population-based strategies, including taxation of unhealthy food items to tackle the epidemic of obesity and type 2 diabetes.”




 Whether it was the courts or the gay pride parades or simply a sign of the times is anybody’s guess but a survey has found that attitudes to homosexuality in India have become increasingly accepting with over a half agreeing having a same-sex partner is acceptable. The Durex Global Sex Survey found that 54% respondents believed that it is ok to have a partner of the same sex while 26% believed it is not acceptable. Forty six percent believed that society is comfortable with consensual sexual activity including homosexuality.
Whether it was the courts or the gay pride parades or simply a sign of the times is anybody’s guess but a survey has found that attitudes to homosexuality in India have become increasingly accepting with over a half agreeing having a same-sex partner is acceptable. The Durex Global Sex Survey found that 54% respondents believed that it is ok to have a partner of the same sex while 26% believed it is not acceptable. Forty six percent believed that society is comfortable with consensual sexual activity including homosexuality.
 In a rare departure from the Jain-Janeu debate that has eclipsed issues in the Gujarat Assembly elections, Congress vice president Rahul Gandhi, one day before his coronation as party president, asked prime minister Narendra Modi on Sunday why 55% of women in the poll bound state are anaemic. Health is rarely an election issue, and women’s health even less so, which is why Gandhi targetting the man who ruled Gujarat for 14 long years before becoming prime minister is a welcome change.
In a rare departure from the Jain-Janeu debate that has eclipsed issues in the Gujarat Assembly elections, Congress vice president Rahul Gandhi, one day before his coronation as party president, asked prime minister Narendra Modi on Sunday why 55% of women in the poll bound state are anaemic. Health is rarely an election issue, and women’s health even less so, which is why Gandhi targetting the man who ruled Gujarat for 14 long years before becoming prime minister is a welcome change.
 Chinese researchers have found that eating cheese, albeit in moderation, may lower the risk of cardiovascular diseases(CVD). The study, published in the European Journal of Nutrition looked at published research on the correlation of cheese and CVD risk – what is called a meta analysis – and found that CVD risk is inversely proportional to cheese consumption. That is, more the latter goes up, higher is the dip in the former.
Chinese researchers have found that eating cheese, albeit in moderation, may lower the risk of cardiovascular diseases(CVD). The study, published in the European Journal of Nutrition looked at published research on the correlation of cheese and CVD risk – what is called a meta analysis – and found that CVD risk is inversely proportional to cheese consumption. That is, more the latter goes up, higher is the dip in the former.
 The ministry has now also started an exercise to ascertain how effective the existing statutory text and pictorial warnings are. “The aim of the exercise is to find out if the new set of pictures and text warnings are impactful or not. Our teams are going to people and taking their suggestions. We are also planning to print the National Tobacco Cessation QuitLine number (
The ministry has now also started an exercise to ascertain how effective the existing statutory text and pictorial warnings are. “The aim of the exercise is to find out if the new set of pictures and text warnings are impactful or not. Our teams are going to people and taking their suggestions. We are also planning to print the National Tobacco Cessation QuitLine number (



 The National AIDS Control Organisation (NACO) on Friday unveiled a even-year National Strategic Plan on HIV/AIDS and STI, 2017-24. The two pillars of the plan are reaching the global 90-90-90 and elimination of transmission of HIV and Syphilis from mother to child by 2020. India is a signatory to the UN strategy of 90-90-90 and is aiming at ending AIDS as a public health threat by 2030. The strategy aims to ensure 90% of people living with HIV know their status, 90% are on ART and 90% have viral suppression.
The National AIDS Control Organisation (NACO) on Friday unveiled a even-year National Strategic Plan on HIV/AIDS and STI, 2017-24. The two pillars of the plan are reaching the global 90-90-90 and elimination of transmission of HIV and Syphilis from mother to child by 2020. India is a signatory to the UN strategy of 90-90-90 and is aiming at ending AIDS as a public health threat by 2030. The strategy aims to ensure 90% of people living with HIV know their status, 90% are on ART and 90% have viral suppression.
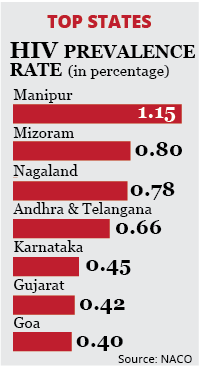 Months after adopting a World Health Organisation (WHO) guideline of treating all HIV+ patients irrespective of their immune status, with a special drug combination, India has registered 50,000 new patients, taking the total number of patents currently receiving anti-retroviral therapy (ART) in the country to 11 lakh.
Months after adopting a World Health Organisation (WHO) guideline of treating all HIV+ patients irrespective of their immune status, with a special drug combination, India has registered 50,000 new patients, taking the total number of patents currently receiving anti-retroviral therapy (ART) in the country to 11 lakh.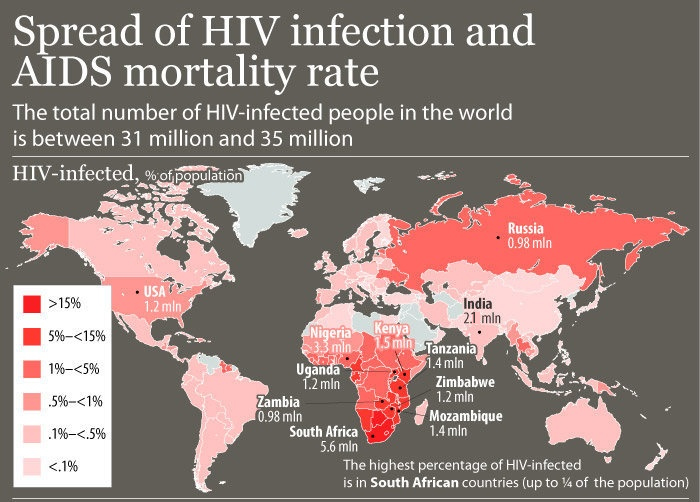

 Bacterial capacity to develop resistance to ampicillin may predate its use in humans and may actually be traced back to the antibiotics use in animals, according to new research published in The Lancet Infectious Diseases.
Bacterial capacity to develop resistance to ampicillin may predate its use in humans and may actually be traced back to the antibiotics use in animals, according to new research published in The Lancet Infectious Diseases.