If you are less than 40 years obese and your friend is balding, your friend may have a higher risk of heart disease.

Male-pattern baldness and premature greying are associated with a more than fivefold risk of heart disease before the age of 40 years, according to research presented at the 69th Annual Conference of the Cardiological Society of India (CSI). Obesity was associated with a fourfold risk of early heart disease.
The congress is being held in Kolkata, India, from 30 November to 3 December. Experts from the European Society of Cardiology (ESC) will present a special programme. “The incidence of coronary artery disease in young men is increasing but cannot be explained by traditional risk factors. Premature greying and androgenic alopecia (male-pattern baldness) correlate well with vascular age irrespective of chronological age and are plausible risk factors for coronary artery disease,” said Dr Sachin Patil, a third year resident at the U.N. Mehta Institute of Cardiology and Research Centre, Ahmedabad, Gujarat, India. ”
This study investigated the association of premature hair greying and balding patterns in young Indian men with coronary artery disease. The study included 790 men aged less than 40 years with coronary artery disease and 1 270 age-matched healthy men who acted as a control group.
The researchers found that young men with coronary artery disease had a higher prevalence of premature greying (50% versus 30%) and male-pattern baldness (49% versus 27%) compared to healthy controls. After adjusting for age and other cardiovascular risk factors, male-pattern baldness was associated with a 5.6 times greater risk of coronary artery disease.
Surprisingly, the study found that while diabetes mellitus, hypertension, family history of premature coronary artery disease, central obesity, higher body mass index and smoking were predictors of coronary artery disease but to a lesser extent than male-pattern baldness, premature greying, and obesity. Principal investigator, Dr Kamal Sharma, associate professor, Department of Cardiology, U.N. Mehta Institute of Cardiology and Research Centre, said: “Baldness and premature greying should be considered risk factors for coronary artery disease. These factors may indicate biological, rather than chronological, age which may be important in determining total cardiovascular risk. Currently physicians use common sense to estimate biological age but a validated scale is needed.”
Professor Marco Roffi, course director of the ESC programme at CSI and head of the Interventional Cardiology Unit, Geneva University Hospital, Geneva, Switzerland, said: “Assessment of risk factors is critical in the prevention and management of cardiovascular disease. Classical risk factors such as diabetes, family history of coronary disease, smoking, sedentary lifestyle, high cholesterol levels and high blood pressure are responsible for the vast majority of cardiovascular disease. It remains to be determined whether potential new risk factors, like the ones described, may improve cardiovascular risk assessment.”





 Indian Council of Medical Research (ICMR) and Zydus have tied up to launch new diagnostic kits, for detection of Japanese Encephalitis Virus (JEV) in mosquito vectors; and the Crimean-Congo Haemorrhagic Fever (CCHF) in sheep, goat and cattle. The kits have been developed by ICMR’s National Institute of Virology (NIV), Pune.
Indian Council of Medical Research (ICMR) and Zydus have tied up to launch new diagnostic kits, for detection of Japanese Encephalitis Virus (JEV) in mosquito vectors; and the Crimean-Congo Haemorrhagic Fever (CCHF) in sheep, goat and cattle. The kits have been developed by ICMR’s National Institute of Virology (NIV), Pune.
 A new global malaria report has sounded warning bells about possible massive under-reporting of malaria in India – to the tune of more than 90%. This after years of malaria having been given the status of a global public health success story, has highlighted the need for developing better surveillance systems on way to its eradication. Drug resistance is one of the main reasons why malaria came back with a vengeance in the 1990s; this has ushered in the era of combination drug therapies to treat Malaria.
A new global malaria report has sounded warning bells about possible massive under-reporting of malaria in India – to the tune of more than 90%. This after years of malaria having been given the status of a global public health success story, has highlighted the need for developing better surveillance systems on way to its eradication. Drug resistance is one of the main reasons why malaria came back with a vengeance in the 1990s; this has ushered in the era of combination drug therapies to treat Malaria.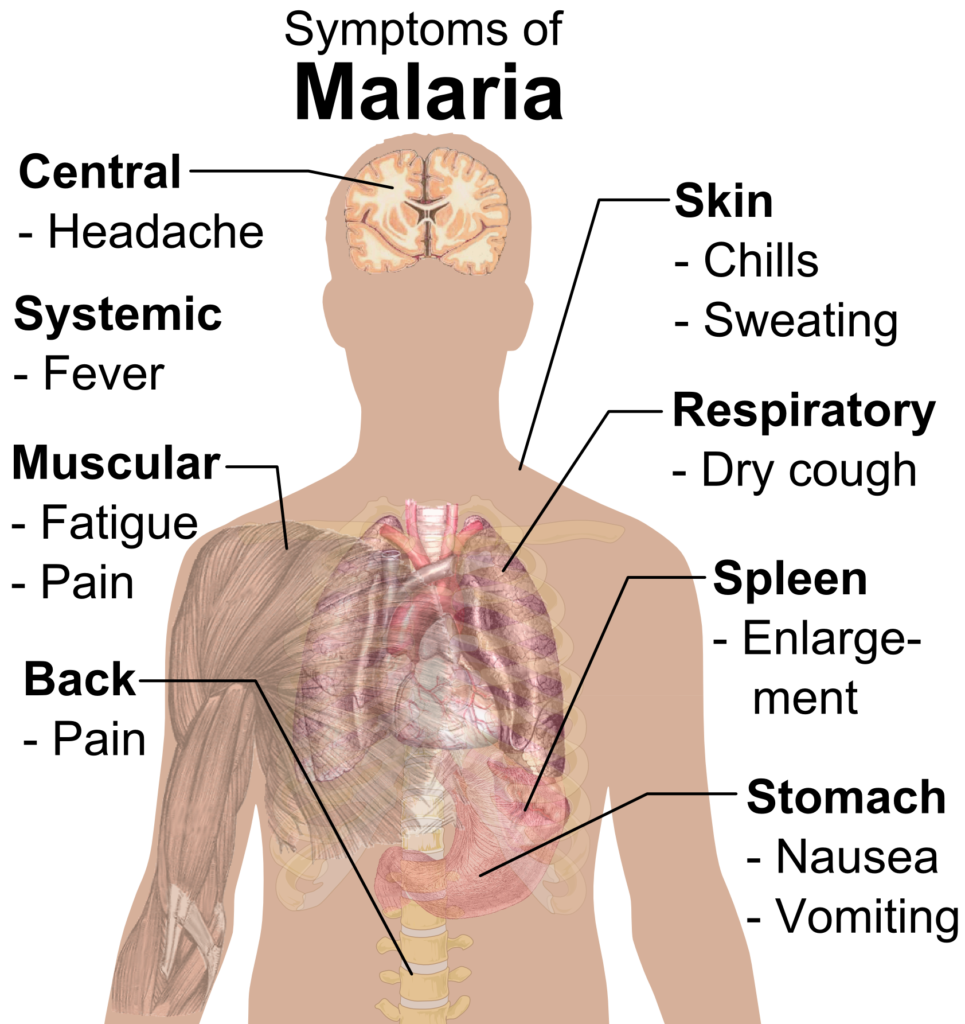 What are the symptoms of malaria?
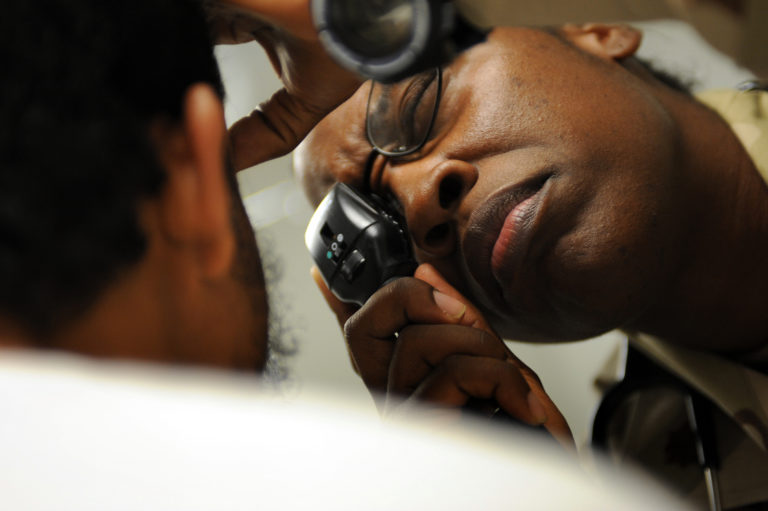
What are the symptoms of malaria? Malaria diagnosis is carried out by microscopic examination of blood films or Rapid Diagnostic Kit tests. Plasmodium vivax malaria is treated with chloroquine and Primaquine. Plasmodium falciparum malaria requires treatment with artemisinin based combination therapy (ACT).
Malaria diagnosis is carried out by microscopic examination of blood films or Rapid Diagnostic Kit tests. Plasmodium vivax malaria is treated with chloroquine and Primaquine. Plasmodium falciparum malaria requires treatment with artemisinin based combination therapy (ACT).
 An estimated 1 in 10 drugs circulating in low- and middle-income countries – what are commonly known as the developing world – is either substandard or falsified, according to new research from the World Health Organization (WHO). However the figure for South Asia is 2%. While the report does not have India-specific figures, earlier surveys have thrown a 5-6% incidence of spurious/substandard drugs in the country.
An estimated 1 in 10 drugs circulating in low- and middle-income countries – what are commonly known as the developing world – is either substandard or falsified, according to new research from the World Health Organization (WHO). However the figure for South Asia is 2%. While the report does not have India-specific figures, earlier surveys have thrown a 5-6% incidence of spurious/substandard drugs in the country.

 The study, published in The Lancet Diabetes and Endocrinology found that 544300 cases of cases were attributable to high BMI (equivalent to 3.9% of all cancers), and 280100 were attributable to diabetes (2%). Global estimates suggest that 422 million adults have diabetes and 2.01 billion adults are overweight or obese. High BMI and diabetes are risk factors for various types of cancer, possibly because of the adverse effects on the body of high insulin, high sugar levels, chronic inflammation, and dysregulated sex hormones such as oestrogen, all of which are associated with these diseases. The study assessed the increase in new cases of 18 cancers based on the prevalence of diabetes and high BMI in 175 countries between 1980 and 2002.
The study, published in The Lancet Diabetes and Endocrinology found that 544300 cases of cases were attributable to high BMI (equivalent to 3.9% of all cancers), and 280100 were attributable to diabetes (2%). Global estimates suggest that 422 million adults have diabetes and 2.01 billion adults are overweight or obese. High BMI and diabetes are risk factors for various types of cancer, possibly because of the adverse effects on the body of high insulin, high sugar levels, chronic inflammation, and dysregulated sex hormones such as oestrogen, all of which are associated with these diseases. The study assessed the increase in new cases of 18 cancers based on the prevalence of diabetes and high BMI in 175 countries between 1980 and 2002.

 Such is the state of mental healthcare in India that President Ramnath Kovind talked earlier this month about India “staring at a mental health epidemic.” Likes of actor Deepika Padukone – now in the news for her controversial film Padmavati – are just beginning to talk here about their own experiences with depression but that of the postpartum variety is yet below the radar of public health discourse.
Such is the state of mental healthcare in India that President Ramnath Kovind talked earlier this month about India “staring at a mental health epidemic.” Likes of actor Deepika Padukone – now in the news for her controversial film Padmavati – are just beginning to talk here about their own experiences with depression but that of the postpartum variety is yet below the radar of public health discourse.
 Air pollution causes 30% of premature deaths in the country, a report released on Monday by the Centre for Science and Environment has revealed. The findings are in line with those of the state level disease burden report released last week that also found that contribution of air pollution to disease burden remains high, with levels of exposure among the highest in the world.
Air pollution causes 30% of premature deaths in the country, a report released on Monday by the Centre for Science and Environment has revealed. The findings are in line with those of the state level disease burden report released last week that also found that contribution of air pollution to disease burden remains high, with levels of exposure among the highest in the world.
 Calling it a “man-made situation” Delhi government has identified the primary sources of pollution as burning of Agricultural residue in neighboring states, motor vehicles emissions, industrial pollution, construction work, bursting of firecrackers, household combustion devices, burning of wood, coal, etc. It could also be a result of burning of fire crackers, a government statement said this evening. This, despite the fact that there was a ban on sale of fire crackers in NCR at the time of Diwali last month.
Calling it a “man-made situation” Delhi government has identified the primary sources of pollution as burning of Agricultural residue in neighboring states, motor vehicles emissions, industrial pollution, construction work, bursting of firecrackers, household combustion devices, burning of wood, coal, etc. It could also be a result of burning of fire crackers, a government statement said this evening. This, despite the fact that there was a ban on sale of fire crackers in NCR at the time of Diwali last month.