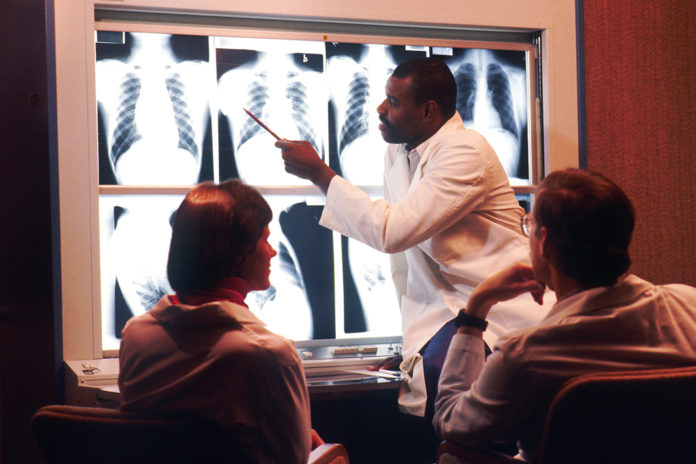
Most post-imaging colorectal cancers arise from errors; radiologist training could help reduce it
Computed Tomography Colonography (CTC), also known as Virtual Colonoscopy is a medical imaging technology used in identifying polyps and colon cancer masses in the large intestine. Polyp is the abnormal growth of tissues found in the inner wall of the colon which may arise from either mucosal layer or submucosal layer.
Eventually they may regress or grow further and can become malignant. The malignant version is called colon cancer and they can occur in any part of the colon.
In a recently published article in the Lancet – Gastroenterology and Hepatology , a systematic review and meta-analysis of post-CT colonography and post-imaging colorectal cancer rates and causes was done to address this gap in understanding
The technique has evolved a great deal since its invention and has become a routine diagnostic procedure in western countries due to its non invasiveness. American Cancer Society recommends CTC as a screening tool. Other recommended modalities include colonoscopy, barium enema and flexible sigmoidoscopy.
The variation in sensitivity and specificity of CTC results when compared to Colonoscopy has resulted in its suboptimal use. Many reports have cited inability of CTC to detect smaller polyps when compared to colonoscopy.The primary concerns are two:
- CTC mainly fails in identifying the smaller lesions of <5mm (Aswakul et al., 2012).
- Colonoscopy overtakes CTC in high risk population as CTC fails for smaller lesions (Broadstock, 2007). The fear was if these small polyps went undetected, they may become colorectal cancers in future.
Interval cancers discovered shortly (eg, 3 years) after a negative colonoscopy are a topic of great clinical interest. Potential explanations for these interval cancers include missed or incompletely resected lesions, or rapidly growing new lesions. Till date the understanding was that most interval cancers after colonoscopy result from missed lesions but data on this is very limited.
In a recently published article in the Lancet – Gastroenterology and Hepatology , a systematic review and meta-analysis of post-CT colonography and post-imaging colorectal cancer rates and causes was done to address this gap in understanding.
The study included randomised, cohort, cross-sectional, or case-control studies published between Jan 1, 1994, and Feb 28, 2017, using CT colonography done according to international consensus standards with the aim of detecting cancer or polyps, and reporting post-imaging colorectal cancer rates or sufficient data to allow their calculation. It excluded studies in which all CT colonographies were done because of incomplete colonoscopy or if CT colonography was done with knowledge of colonoscopy findings.
Data from 19867 patients (aged 18–96 years; of 11590 with sex data available, 6532 [56%] were female) between March, 2002, and May, 2015 was evaluated. At a mean of 34 months’ follow-up (range 3–128·4 months), CT colonography detected 643 colorectal cancers. 29 post-imaging colorectal cancers were subsequently diagnosed. The pooled post-imaging colorectal cancer rate was 4·42 (95% CI 3·03–6·42) per 100 cancers detected, corresponding to 1·61 (1·11–2·33) post-imaging colorectal cancers per 1000 CT colonographies or 0·64 (0·44–0·92) post-imaging colorectal cancers per 1000 person-years. 17 (61%) of 28 post-imaging colorectal cancers were attributable to perceptual error and were visible in retrospect.
The study concluded that CT colonography does not lead to an excess of post-test cancers relative to colonoscopy within 3–5 years, and the low 5-year post-imaging colorectal cancer rate confirms that the recommended screening interval of 5 years is safe. Since most post-imaging colorectal cancers arise from perceptual errors, radiologist training and quality assurance could help to reduce post-imaging colorectal cancer rates.