A drug called nafamostat mesylate could prevent blood vessel leakage in severe dengue haemorrhagic fever
A drug for dengue haemorrhagic fever may be on the horizon.
Researchers have discovered that tryptase, an enzyme in human cells that acts like scissors to cut up nearby proteins, is responsible for blood vessel leakage in severe dengue haemorrhagic fever. The finding suggests a possible new treatment strategy using the tryptase inhibitor, nafamostat mesylate, for severe dengue disease – a potentially fatal condition.
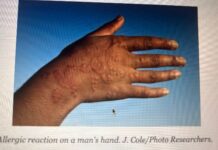
While most patients experience dengue fever or a mild form of the disease, a small percentage develops dengue haemorrhagic fever (DHF), the more severe form of dengue wherein blood ‘leaks’ from ruptured blood vessels. This can lead to dengue shock syndrome (DSS) – the final stage of DHF – where the circulatory system fails, sending the body into bleeding and shock, which is fatal without prompt treatment. Presently no targeted treatments are available to prevent hemorrhaging or reverse shock in infected patients.
Nafamostat mesylate, a clinically-approved inhibitor of tryptase with a good safety profile… They found that administration of this drug, which is already used for the treatment of certain bleeding complications in some countries, prevented vascular leakage
“We discovered that, in severe cases, a particular enzyme called tryptase cuts the proteins that act as seals between blood vessel cells, resulting in blood vessel leakage and shock during dengue infection,” said Assistant Professor Ashley St. John, from Duke-NUS’ Emerging Infectious Diseases Programme, corresponding author of the study.
Nafamostat mesylate, a clinically-approved inhibitor of tryptase with a good safety profile, was tested using preclinical models. They found that administration of this drug, which is already used for the treatment of certain bleeding complications in some countries, prevented vascular leakage in the dengue model. Even delayed treatment with the drug was significantly effective in reducing dengue vascular leakage in a preclinical model of severe disease. The team also observed tryptase levels were very high in the blood of severe dengue patients who experienced DHF/DSS, but low in patients who easily recovered, affirming the link between high levels of the enzyme and severe dengue disease.
“This timely study by our researchers not only holds out hope for a promising new strategy to treat severe dengue disease, but could also have broader implications for the treatment of other haemorrhagic diseases,” said Professor Patrick Casey, Senior Vice Dean for Research at Duke-NUS.
The study authors next plan to conduct clinical trials in humans.