For three days now, vaccinators in vans, on foot and in some areas even in boats have been fanning out in 190 districts of the country to ensure that children and pregnant women left out of the routine immunisation exercise are covered. The weeklong third phase of Intensified Mission Indradhanush (IMI) started on December 7 and will go on till 13.

Prime minister Narendra Modi in October this year, IMI is targetted at every child under two years of age. The special drive focuses on improving immunization coverage in select districts and cities to ensure full immunization to more than 90% by December 2018. The achievement of full immunisation under Mission Indradhanush to at least 90% coverage was to be achieved by 2020 earlier. With the launch of IMI, achievement of the target has now been advanced. Mission Indradhanush recently came in for rich praise in a global pneumonia/diarrhoea report card drawn up by Johns Hopkins Bloomberg School of Public Health and other partners.
Four phases of Mission Indradhanush have reached to more than 2.53 crore children and 68 lakh pregnant women. Vaccination is accepted the world over as one of the most effective preventive measures and one of the best ways to prevent under five child mortality. Yet only 62% of children are fully immunised says data from the National Family Health Survey 4. There are wide variations between states – the coverage is 38.2% in Arunachal Pradesh and 82% in Kerala.
The vaccines covered in the universal immunisation programme include BCG, hepatitis B, polio, diphtheria, pertussis and tetanus, measles-rubella, Japanese Encephalitis (in endemic areas), pneumonia and rotavirus. “It is for the states to devise strategies best suited to reach the target population in chosen districts – for example in riverine districts like Dhubri in Assam boats may be pressed into service. There is one mobile vaccination unit – commonly known as vaccine vans – in Srawasti district of Uttar Pradesh. In North 24 Parganas of West Bengal where there is a substantial Muslim population, clerics have been roped in to take the message across,” said a senior health ministry official.
For IMI the Union ministry of health is leaving no stone unturned with daily monitoring happening through officers whatsapp groups and additional resources been given to states to reach the target. Items like vaccine vans or refrigerators to store vaccines states have been given for IMI will henceforth become a part of the routine immunisation programme – that in fact is one of the key differences from Mission Indradhanush as it was since its launch on December 25, 2014. IMI will also award states and districts reaching more than 90% coverage. Targets have been set at 90% rather than 100 because it is a fact accepted in public health globally that the last 10% is usually the hardest to achieve and also requires far higher resource commitment.




 What is influenza?
What is influenza? There is, actually. The disease usually picks up in the winter months starting October and lasts upto March of every year. It is a contagious disease which means affected individuals can pass on the infection to people who come in contact with them. It can sometimes lead to more serious complications like sinus and ear infections, pneumonias, life threatening sepsis etc. Young children below 5 years of age, senior citizens, pregnant women, people with preexisting chronic diseases (like Diabetes, Tuberculosis,COPD, asthma etc) and smokers are particularly at risk of serious infection due to weakened immune system. High levels of household and ambient air pollution are also associated with increased complication rates.
There is, actually. The disease usually picks up in the winter months starting October and lasts upto March of every year. It is a contagious disease which means affected individuals can pass on the infection to people who come in contact with them. It can sometimes lead to more serious complications like sinus and ear infections, pneumonias, life threatening sepsis etc. Young children below 5 years of age, senior citizens, pregnant women, people with preexisting chronic diseases (like Diabetes, Tuberculosis,COPD, asthma etc) and smokers are particularly at risk of serious infection due to weakened immune system. High levels of household and ambient air pollution are also associated with increased complication rates. The best way to prevent the illness and its spread is by receiving a shot of Flu Vaccine which is recommended for everyone above the age of 6months of age. The Flu vaccine is produced from the influenza virus that has been weakened or inactivated. Since there are variations, known as “strains,” in the flu virus from year to year, and place to place, vaccines protect against the three or four strains that research shows will be most common during the upcoming season. These are known as trivalent (three-sided) or quadrivalent (four-sided) vaccines. It is usually administered in the form of injection. It takes about two weeks for the antibodies against flu to develop.
The best way to prevent the illness and its spread is by receiving a shot of Flu Vaccine which is recommended for everyone above the age of 6months of age. The Flu vaccine is produced from the influenza virus that has been weakened or inactivated. Since there are variations, known as “strains,” in the flu virus from year to year, and place to place, vaccines protect against the three or four strains that research shows will be most common during the upcoming season. These are known as trivalent (three-sided) or quadrivalent (four-sided) vaccines. It is usually administered in the form of injection. It takes about two weeks for the antibodies against flu to develop.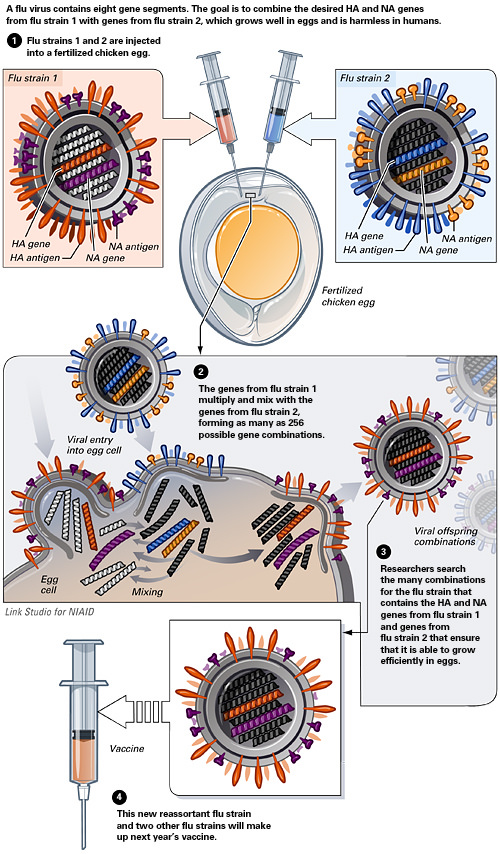



 Researchers at the University College London have found. A UCL study, published in PLOS Medicine, analysed cohort data from three eastern European countries and found that heart disease incidence is more likely among people who rarely see their friends and relatives, are single, unemployed, less wealthy, and have depression-like symptoms. The researchers focused on eastern European countries because heart disease rates are higher there than anywhere else in the world.
Researchers at the University College London have found. A UCL study, published in PLOS Medicine, analysed cohort data from three eastern European countries and found that heart disease incidence is more likely among people who rarely see their friends and relatives, are single, unemployed, less wealthy, and have depression-like symptoms. The researchers focused on eastern European countries because heart disease rates are higher there than anywhere else in the world.




 Researchers at the Temple University administered canola oil (also known as rapeseed oil) to mouse and studied its effects on a variety of neurological aspects including Alzheimer’s Disease pathogenesis (process by which a disease happens). “In conclusion, our investigation demonstrates for the first time to the best of our knowledge a negative effect of the chronic consumption of canola oil on memory, synaptic integrity and Aβ 42/40 ratios in a mouse model of AD (Alzheimer’s Disease). The translational value of our findings lies in the observation that this type of oil supplementation can influence some of the most important features of the AD pathological phenotype,” they concluded in the study that was published in Scientific Reports. In short they found that the neurological incidents leading to AD are hastened by rapeseed oil.
Researchers at the Temple University administered canola oil (also known as rapeseed oil) to mouse and studied its effects on a variety of neurological aspects including Alzheimer’s Disease pathogenesis (process by which a disease happens). “In conclusion, our investigation demonstrates for the first time to the best of our knowledge a negative effect of the chronic consumption of canola oil on memory, synaptic integrity and Aβ 42/40 ratios in a mouse model of AD (Alzheimer’s Disease). The translational value of our findings lies in the observation that this type of oil supplementation can influence some of the most important features of the AD pathological phenotype,” they concluded in the study that was published in Scientific Reports. In short they found that the neurological incidents leading to AD are hastened by rapeseed oil.
 India has eliminated trachoma, a chronic infective disease of the eye and is the leading cause of infective blindness globally. The National Trachoma Prevalence Surveys and the Trachoma Rapid Assessment Surveys conducted by experts from the All India Institute of Medical Sciences found an overall prevalence of 0.7%. The WHO limit for elimination is 5%.
India has eliminated trachoma, a chronic infective disease of the eye and is the leading cause of infective blindness globally. The National Trachoma Prevalence Surveys and the Trachoma Rapid Assessment Surveys conducted by experts from the All India Institute of Medical Sciences found an overall prevalence of 0.7%. The WHO limit for elimination is 5%.
 It is flu season once more and as numbers in the USA cause panic – in India winter is yet to kick in and the influenza virus is not having a field day just yet – experts have called for a universal flu vaccine. The flu vaccine which is really the cornerstone of influenza prevention has to be updated every year as per World Health Organisation updates in February on the circulating strain.
It is flu season once more and as numbers in the USA cause panic – in India winter is yet to kick in and the influenza virus is not having a field day just yet – experts have called for a universal flu vaccine. The flu vaccine which is really the cornerstone of influenza prevention has to be updated every year as per World Health Organisation updates in February on the circulating strain. FLU VACCINE
FLU VACCINE Flu Vaccine Is The Best Protection
Flu Vaccine Is The Best Protection