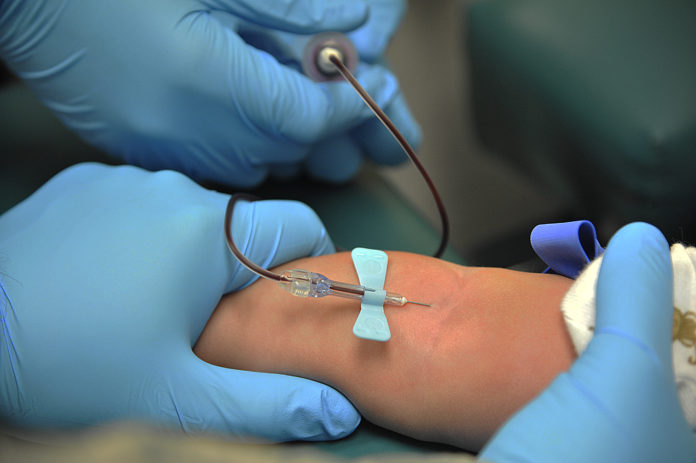
The Peripherally Inserted Central Catheter (PICC) is used to deliver drugs/nutrition, but exposes patients to complications
An intravenous line very commonly used to deliver medications/nutrition in an ICU may be grossly overused, exposing patients to unnecessary risks. The Peripherally Inserted Central Catheter (PICC) in just a decade since its arrival, has become the go-to device for intravenous care.
One in three short-term PICC patients also had serious kidney problems that could make them potential dialysis candidates, the study also shows.
But a new study finds that one in every four times a PICC gets inserted, the patient didn’t need it long enough to justify the risks that it can also pose. In fact, in just the five days or less that they had a PICC implanted in their vein, nearly one in ten of these patients suffered a blocked line, an infection, a blood clot or another complication linked to the device.
One in three short-term PICC patients also had serious kidney problems that could make them potential dialysis candidates, the study also shows. They face special risks from the devices, which can harm blood vessels and jeopardize a patient’s ability to receive dialysis later, if their kidneys fail.
The study, published in the February issue of Journal of Hospital Medicine is based on data from 52 hospitals around the state of Michigan taking part in a massive quality improvement and patient safety effort. It’s a detailed analysis of records from 15,397 PICC placements over a two-year period from 2014 to 2016, just before and after guidelines for safe and appropriate PICC use made their debut.
The study highlights the need for efforts to reduce short-term use of PICCs and help medical care teams understand current practice and consider other alternatives for short-term IV access that pose less risk.
“When PICCs first came out, they became an ‘easy button’ for vascular access, and the safety issues weren’t recognized. Now the dynamics have changed, and we need to be more thoughtful with their us,” says David Paje University of Michigan hospitalist who led the research team.







