New guideline recommends weight loss strategies for sleep apnea patients
The latest guideline on management of adult obstructive sleep apnea focuses on weight management as a treatment strategy. It has been published in the American Journal of Respiratory and Critical Care Medicine.
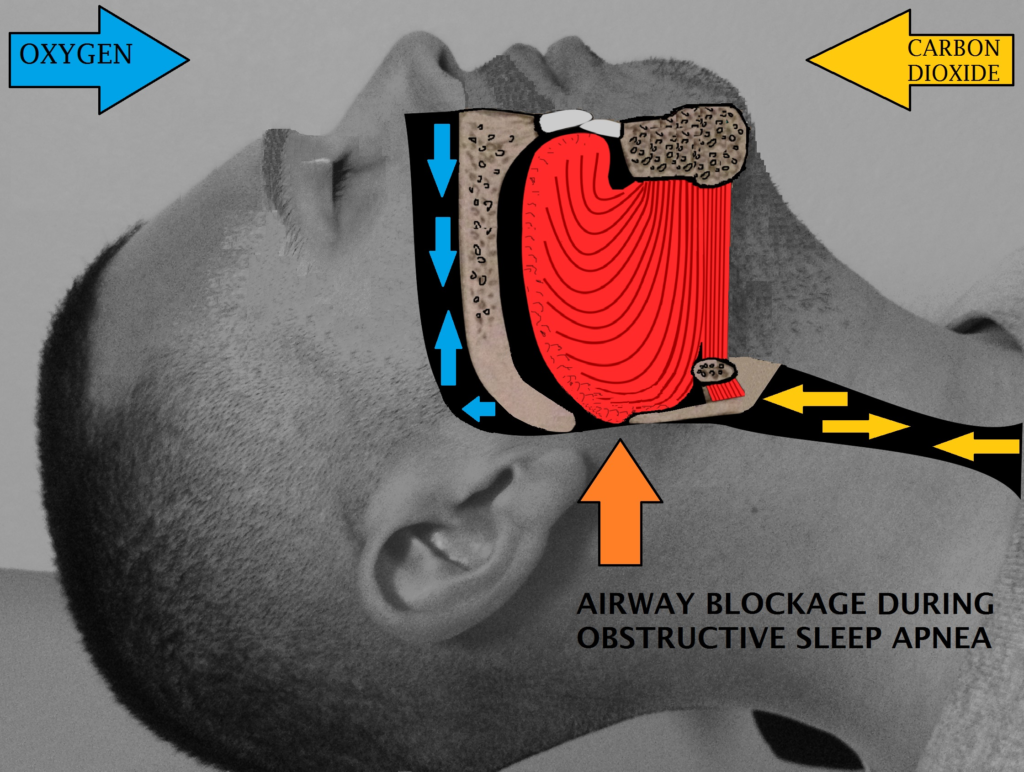
OSA or obstructive sleep apnea is a common condition that occurs when air passing through the breathing passage becomes completely shut leading to temporary cessation of respiration. It is a condition in which respiration is disrupted repeatedly during sleep, and a person wakes up from sleep.
Being overweight or obese is a strong risk factor for OSA, and weight loss can often reduce the severity of OSA.
Gastric banding was not found to be more effective in reducing OSA severity than lifestyle interventions that result in weight loss
A 20 member panel of American Thoracic Society – which included sleep, pulmonary, weight management and behavioral experts, as well as three patients looked at different studies and formulated new guidelines for OSA.
BMI which is a measure of fatness or thinness of an adult person was used in formulation of these guidelines. BMI is calculated by dividing weight in kilograms (kg) by his or her height in meters squared.
For patients with OSA who are overweight or obese (body mass index – BMI around 25 kg/m2 ) the panel:
• Recommended participation in a comprehensive lifestyle intervention program that includes a reduced calorie diet, exercise/increased physical activity and behavioral counseling
• Suggested that in the absence of a comprehensive program, participation in a diet and exercise program is recommended, together or individually
For patients with OSA who have a BMI around 27 kg/m2 and whose weight has not improved despite participating in a comprehensive program and who have no contraindications to pharmacotherapy such as active cardiovascular disease, the panel:
• Suggested an evaluation for anti-obesity pharmacotherapy
• The panel defined active cardiovascular diseases as “myocardial infarction or cerebrovascular accident within the past six months, uncontrolled hypertension, life-threatening arrhythmias or decompensated congestive heart failure.”
For patients with OSA who have a BMI around 35 kg/m2 and whose weight has not improved despite participating in a comprehensive weight loss lifestyle intervention program–and who have no contraindications, the panel:
• Suggested referral for bariatric surgery evaluation
In the only available well-controlled trials, gastric banding was not found to be more effective in reducing OSA severity than lifestyle interventions that result in weight loss.
The panel also noted that weight loss, either through lifestyle changes or bariatric surgery, has benefits beyond reducing OSA severity, which includes prevention of type 2 diabetes, improved glycemic control in those with type 2 diabetes, lower blood pressure and improved quality of life.
“This guideline demonstrates that weight loss provides a distinct benefit to OSA patients, but many patients may not know about how to achieve these benefits because their health care provider has not had an in-depth discussion about proven methods to achieve weight loss with them,” said panel co-chair Sanjay R. Patel, MD, professor of medicine and medical director of the sleep laboratory at the University of Pittsburgh Medical Center.